Purpose

Introduction
Vector-borne diseases are found at almost every travel destination. Because few vaccines are available to protect travelers, the best way to prevent vector-borne diseases is to avoid being bitten by ticks and insects, including mosquitoes, fleas, chiggers, and flies, that transmit pathogens that cause disease. Travel medicine specialists should advise travelers to use repellents and take other precautions to prevent bites.
Elevation and arboviral disease risk
Mosquito-borne diseases are most often reported from tropical and subtropical areas, with risk declining as elevation increases. However, some vector species of mosquitoes are established at high elevations. West Nile and Usutu viruses were reported to be circulating in wildlife sentinel animals in the Italian Alps in 2005; however, no human cases were detected. Japanese encephalitis virus infections were detected in mosquitoes, pigs, and humans in Tibet, China, in the Nyingchi District at elevation 3,100 m (10,170 ft).
Vaccine options and malaria prophylaxis
Vaccines are currently available to protect against 4 vector-borne diseases in U.S. travelers: chikungunya, Japanese encephalitis, tick-borne encephalitis, and yellow fever (see: Chikungunya, Japanese Encephalitis, Tick-Borne Encephalitis; and Yellow Fever chapters). For these travel-associated, vector-borne diseases, no specific antiviral treatments are available, and therapy consists of supportive care and management of complications.
No vaccines are available in the United States for other mosquito-borne diseases (e.g., filariasis, West Nile encephalitis, Zika); tickborne diseases (e.g., Lyme borreliosis, relapsing fever); sand fly-borne diseases (e.g., cutaneous or visceral leishmaniasis); tsetse fly-borne diseases (e.g., African trypanosomiasis); or blackfly-borne diseases (e.g., onchocerciasis [river blindness]). No pre-exposure prophylaxis is available for vector-borne diseases other than malaria. The effectiveness of malaria prophylaxis is variable, depending on patterns of drug resistance, bioavailability, individual behavior, and compliance with medication (see Yellow Fever Vaccine and Malaria Prevention Information, by Country and Malaria chapters).
Insect repellants
Topical repellents
Insect repellents registered by the Environmental Protection Agency (EPA) have been proven effective in reducing biting by insects such as mosquitoes and sand flies, as well as other arthropods, such as ticks and mites. EPA-registered products are considered safe when used as directed, even for pregnant and breastfeeding women. CDC has evaluated information published in peer-reviewed scientific literature and data available from EPA to identify several types of EPA-registered products that safely and effectively prevent insect bites. Products containing the following active ingredients typically provide reasonably long-lasting protection:
- DEET (chemical name: N,N-diethyl-m-toluamide or N,N-diethyl-3-methyl-benzamide)
- Picaridin (KBR 3023 and icaridin outside the United States; chemical name: 2-[2-hydroxyethyl]-1-piperidinecarboxylic acid 1-methylpropyl ester)
- Oil of lemon eucalyptus (OLE) or PMD (chemical name: para-menthane-3,8-diol, the synthesized version of OLE); CDC does not recommend using "pure" oil of lemon eucalyptus (an essential oil that is not formulated) as a repellent because it has not undergone validated testing for safety and efficacy and is not registered with EPA as an insect repellent; in general, parents should not use products containing OLE or PMD on children <3 years old to avoid potential allergic skin reactions
- IR3535 (chemical name: 3-[N-butyl-N-acetyl]-aminopropionic acid, ethyl ester)
- 2-undecanone (chemical name: methyl nonyl ketone)
EPA characterizes the active ingredients DEET and picaridin as "conventional" repellents. The biopesticide repellents (OLE, PMD, IR3535, and 2-undecanone) are derived from, or are synthetic versions of, natural materials.
Travelers can find the right insect repellent for their needs by searching the EPA website Find the Repellent That Is Right for You and the National Pesticide Information Center website, Choosing and Using Insect Repellents. Recommendations from these websites are based on peer-reviewed journal articles and scientific studies and data submitted to regulatory agencies.
Ideally, travelers should purchase repellents before departing the United States. A wide variety of repellents are available at camping, sporting goods, and military surplus stores. When purchasing repellents overseas, travelers should look for the active ingredients specified above on the product labels.
Efficacy
Published data indicate that repellent efficacy and duration of protection vary considerably among products and among arthropod species. Product efficacy and duration of protection are also markedly affected by ambient temperature, level of activity, amount of perspiration, exposure to water, being rubbed off during activities, and other factors.
In general, higher concentrations of active ingredients provide longer duration of protection, regardless of the active ingredient. Products with <10% active ingredient might offer only limited protection, often 1–2 hours. Products that offer sustained-release or controlled-release (microencapsulated) formulations, even with lower active ingredient concentrations, might provide longer protection times. Studies suggest that DEET efficacy tends to peak at a concentration of approximately 50% and that concentrations above that do not offer a marked increase in protection time against mosquitoes. Regardless of the product used, if travelers start getting bitten, they should reapply but not more often than the label allows.
The effectiveness of non-EPA-registered insect repellents, including some natural repellents, is unknown, and travelers should avoid using them (see EPA webpage on Repellents: Protection Against Mosquitoes, Ticks and Other Arthropods). Ingestion of vitamin B or garlic and wearing sound-emitting devices or repellent-impregnated wristbands are ineffective.
Repellents and sunscreen
Repellents applied according to label instructions can be used with sunscreen with no reduction in repellent activity (see Sun Exposure in Travelers chapter). However, limited data show that DEET-containing insect repellents applied over sunscreen decrease the sun protection factor (SPF) of the sunscreen by one-third.
Travelers should avoid products that combine sunscreen with repellents because sunscreen might need to be reapplied more often and in larger amounts than what is needed for the repellent component to provide protection from biting insects. In general, travelers should use separate products, apply sunscreen first, and then apply the repellent. Because SPF decreases when a DEET-containing insect repellent is used, travelers might need to reapply sunscreen more frequently. Travelers must remember to use both sunscreen and insect repellents according to the manufacturer's instructions for each.
Spatial repellents
Spatial repellents, including aerosol insecticide sprays, vaporizing mats, and mosquito coils, contain active ingredients (e.g., metofluthrin, allethrin) that people can use to protect against insect bites. Spray aerosols can help clear mosquitoes from larger spaces, while coils and spatial repellents repel mosquitoes from more circumscribed areas.
Although many of these products have repellent or insecticidal activity under certain conditions, they have not yet been adequately evaluated in peer-reviewed studies for efficacy in preventing vector-borne diseases. Travelers should supplement use of these products with an EPA-registered repellent on skin or clothing and by using mosquito nets in areas where vector-borne diseases are a risk or biting arthropods are noted.
Some products available internationally might contain pesticides that are not registered for use in the United States. Conversely, travelers intending to bring their own spatial repellents should make sure the repellents are legal for use at their destination. Travelers should consult the U.S. embassy website in the destination country. Advise travelers to use spatial repellents with caution and to avoid direct inhalation of spray or smoke.
Use on clothing and gear
Travelers can treat clothing, hats, shoes, mosquito nets, outerwear, and camping gear with permethrin for added protection. Permethrin is a highly effective insecticide, acaricide (pesticide that kills ticks and mites), and repellent. At a concentration of 0.5%, permethrin-treated clothing repels and kills ticks, chiggers, mosquitoes, and other biting and nuisance arthropods. Clothing and other items must be treated 24–48 hours before packing for travel to allow them to dry. As with all pesticides, travelers should always follow the label instructions.
EPA-registered products with permethrin for the treatment of clothing and gear are marketed under several brand names, including Sawyer, Repel, and Ultrathon. Alternatively, clothing pre-treated with permethrin is commercially available and marketed to consumers in the United States as Insect Shield, BugsAway, and Insect Blocker.
Permethrin-treated materials retain repellency or insecticidal activity after repeated launderings but should be retreated as described on the product label to provide continued protection. Clothing treated before purchase is labeled for efficacy through many launderings. Clothing treated with the other repellent products described above (e.g., DEET) provides protection from biting arthropods but will not last through washing and will require more frequent application.
Precautions
Box 3.6.1 contains precautions that healthcare professionals can share with travelers regarding the use of insect repellents. Severe reactions to insect repellents are rare. If a traveler experiences a rash or other reaction (e.g., itching, swelling) from a repellent, they should wash off the product using mild soap and water and discontinue its use. Travelers seeking health care because of a reaction to a repellent should take the product container with them to the doctor's office. Reactions associated with insect repellent use are outlined in MedlinePlus.
Permethrin should never be applied to the skin but only to clothing, mosquito nets, or other fabrics as directed on the product label.
Box 3.6.1
Children and pregnant women
Certain insect repellent products containing OLE as their sole active ingredient at concentrations of ≤30% can be used on children <3 years of age; parents should always read the product label before use. Insect repellents containing DEET, picaridin, IR3535, and 2-undecanone can be used on children without age restriction (see EPA webpage on Using Insect Repellents Safely and Effectively with Children). Travelers can protect infants from insect bites by dressing them in clothing that covers their arms and legs, by covering strollers and baby carriers with mosquito netting, and by using appropriate insect repellent. Other than the safety tips listed above, EPA does not recommend any additional precautions for using registered repellents on children or on women who are pregnant or lactating.
Additional methods of arthropod bite prevention
Travelers can reduce their risk for bites from mosquitoes, ticks, fleas, sand flies, and other arthropods by using EPA-registered insect repellents. Travelers should also minimize areas of exposed skin by wearing long-sleeved shirts, long pants, boots, and hats. Tucking in shirts, tucking pants into socks, and wearing closed shoes instead of sandals also reduce risk. Additional prevention techniques are provided below.
Mosquitoes
More than 3,700 different mosquito species live worldwide, and each has specific biting behaviors; some species have local and regional variations, meaning biting behaviors might not be uniform throughout the distribution range of a specific species. Mosquitoes bite throughout the day and night, although each species tends to have peak activity at certain times.
The peak biting activity of Aedes aegypti (the primary vector for chikungunya, dengue, Mayaro, yellow fever, and Zika) is after sunrise (dawn) and at sunset (dusk). By contrast, peak biting activity for Culex quinquefasciatus (a vector for filariasis; Japanese, St. Louis, and West Nile encephalitis; and Usutu) is typically after sunset, usually between 10 and 11 p.m. The biting activity of Anopheles mosquitoes, the primary vectors for malaria worldwide, varies with the species. In general, peak biting activity for Anopheles species tends to be during the night or evening hours.
Avoiding peak biting activity periods minimizes the chances of exposure to vector-borne diseases. Although some mosquito species can roughly be described as day-biters and others as nocturnal feeders, regional variations and overlap in feeding times means that travelers need to be cautious about mosquito bites at all times of day and night in regions where mosquito-borne diseases are a risk (see Table 3.6.1).
As much as possible, travelers should avoid visiting areas with active outbreaks of mosquito-borne diseases. The CDC Travelers' Health website provides updates on regional disease transmission patterns and outbreaks.
Table 3.6.1: Peak biting activity times for vectors of mosquito-borne diseases
| Vector | Mosquito-Borne Disease | Peak Biting Periods |
|---|---|---|
| Aedes aegypti | Chikungunya, dengue, Mayaro, yellow fever, Zika | Dawn and dusk |
| Aedes albopictus | Chikungunya, dengue, Mayaro, Zika | Dawn and dusk |
| Culex quinquefasciatus | Filariasis; Japanese, St. Louis, and West Nile encephalitis; Usutu | Late evening (10–11 p.m.) |
| Anopheles | Malaria | Night and evening |
Biting midges
Biting midges, also known as no-see-ums, are active in the daytime and evening and are responsible for the transmission of pathogens such as Oropouche virus. EPA-registered repellents that are labeled for flies, biting flies, and no-see-ums are effective for repelling biting midges. Screens that are commonly used as insect barriers do not have holes small enough to prevent biting midges from getting inside. To prevent biting midges from entering the home, mesh screens measuring 20x20 should be installed.
Ticks
Hiking, camping, and hunting are examples of activities that could bring travelers in close contact with ticks. Travelers should avoid wooded and brushy areas with high grass and leaf litter and stay in the center of hiking trails.
Figure 3.6.1 provides instructions on how to remove attached ticks. Counsel travelers who develop rash or fever within several weeks of removing a tick to see a doctor; travelers should provide details (if known) about the bite, including when and where it occurred.
Figure 3.6.1
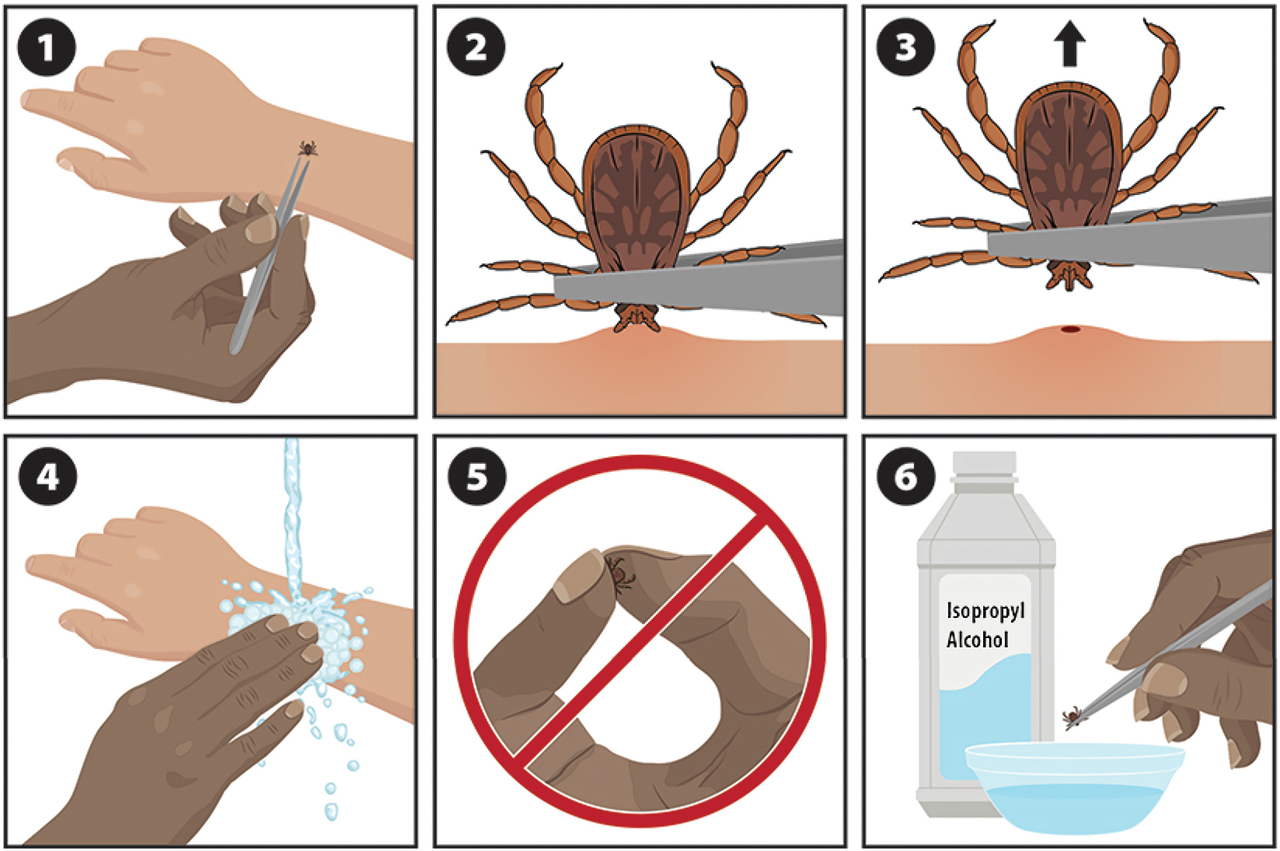
Centers for Disease Control and Prevention
Notes
(1) If a tick is attached to the skin, remove it as soon as possible.
(2) Several tick removal devices are available on the market, but fine-tipped tweezers also work very well.
(3) Using fine-tipped tweezers, grasp the tick as close to the surface of the skin as possible. Pull upward with steady, even pressure without twisting or jerking the tick; twisting or jerking can cause the mouthparts of the tick to break off in the skin. If the mouthparts of the tick break off in the skin, and they can be removed easily, remove them with tweezers. If the mouthparts cannot be removed easily, leave them alone and allow the skin to heal.
(4) After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.
(5) Never crush a tick with your fingers.
(6) Dispose of live ticks by placing them in alcohol or a sealed container, wrapping them tightly with tape, or flushing them down the toilet.
Fleas
Flea bites often occur on the lower legs and feet. Travelers can protect these areas of the body by wearing long socks and pants. In addition, travelers should not feed or pet stray or wild animals. For more on flea bite prevention techniques, see Preventing Fleas. For more on the importance of avoiding animals while traveling, see Zoonotic Exposures: Bites, Scratches, and Other Hazards chapter.
Sand flies
Sand flies are most active during dawn and dusk. If possible, travelers should limit outdoor activities during those times.
Tsetse flies
To protect against tsetse fly bites, travelers should wear long-sleeved shirts and long pants that are neutral-colored because tsetse flies are attracted to bright or dark colors, particularly blue and black. Tsetse flies can bite through lightweight clothing, so medium-weight clothing provides better protection. Travelers should avoid areas with heavy vegetation, particularly during the hottest times of day; although tsetse flies are less active during these times, they tend to bite if disturbed. Permethrin-impregnated clothing and insect repellent have not been proven to be effective against tsetse flies.
Bed bugs
Bed bugs have not been shown to transmit disease to humans. A recent surge in bed bug infestations worldwide, particularly in high-income countries, is thought to be related to international travel, changes in pest-control strategies in hotels and housing, and insecticide resistance. Bed bug infestations have been reported in hotels, theaters, and locations where people congregate, even in the workplace, dormitories, and schools.
Bed bugs are small, flat insects that are reddish-brown in color, wingless, and range from 1 to 7 mm in length. Bed bug bites can produce strong allergic reactions and considerable emotional stress. Bed bugs can be transported in luggage and on clothing and by transporting personal belongings in contaminated transport vehicles.
Travelers can take measures to avoid bed bug bites and avoid transporting them in luggage and clothing (Box 3.6.2). Prevention is by far the most effective and inexpensive way to protect oneself from these pests. The cost associated with ridding a personal residence of bed bugs is considerable, and efforts at controlling bed bugs are often not immediately successful, even when conducted by professionals.
Box 3.6.2
- Achee, N. L., Perkins, T. A., Moore, S. M., Liu, F., Sagara, I., Van Hulle, S., . . . Grieco, J. P. (2022). Spatial repellents: The current roadmap to global recommendation of spatial repellents for public health use. Current Research in Parasitology & Vector-Borne Diseases, 3, 1–9. https://www.doi.org/10.1016/j.crpvbd.2022.100107
- Agius, P. A., Cutts, J. C., Han Oo, W., Thi, A., O’Flaherty, K., Zayar Aung, K., . . . Fowkes, F. J. I. (2020). Evaluation of the effectiveness of topical repellent distributed by village health volunteer networks against Plasmodium spp. infection in Myanmar: A stepped-wedge cluster randomised trial. PLoS Medicine, 17(8), e1003177. https://www.doi.org/10.1371/journal.pmed.1003177
- Agumba, S., Moshi, V., Muchoki, M., Omondi, S., Kosgei, J., Walker, E. D., . . . Ochomo, E. (2024). Experimental hut and field evaluation of a metofluthrin-based spatial repellent against pyrethroid-resistant Anopheles funestus in Siaya County, western Kenya. Parasites & Vectors, 17(1), 6. https://www.doi.org/10.1186/s13071-023-06096-2
- Gabaldón Figueira, J. C., Wagah, M. G., Adipo, L. B., Wanjiku, C., & Maia, M. F. (2023). Topical repellents for malaria prevention. The Cochrane Database of Systematic Reviews, 8(8), CD015422. https://www.doi.org/10.1002/14651858.CD015422.pub2
- Goodyer, L. I., Croft, A. M., Frances, S. P., Hill, N., Moore, S. J., Onyango, S. P., . . . Debboun, M. (2010). Expert review of the evidence base for arthropod bite avoidance. Journal of Travel Medicine, 17(3), 182–192. https://www.doi.org/10.1111/j.1708-8305.2010.00402.x
- Lupi, E., Hatz, C., & Schlagenhauf, P. (2013). The efficacy of repellents against Aedes, Anopheles, Culex and Ixodes spp.: A literature review. Travel Medicine and Infectious Disease, 11(6), 374–411. https://www.doi.org/10.1016/j.tmaid.2013.10.005
- Morrison, A. C., Reiner, R. C., Jr, Elson, W. H., Astete, H., Guevara, C., Del Aguila, C., . . . Achee, N. L. (2022). Efficacy of a spatial repellent for control of Aedes-borne virus transmission: A cluster-randomized trial in Iquitos, Peru. Proceedings of the National Academy of Sciences of the United States of America, 119(26), e2118283119. https://www.doi.org/10.1073/pnas.2118283119
- Murphy, M. E., Montemarano, A. D., Debboun, M., & Gupta, R. (2000). The effect of sunscreen on the efficacy of insect repellent: A clinical trial. Journal of the American Academy of Dermatology, 43(2 Pt 1), 219–222. https://www.doi.org/10.1067/mjd.2000.107960
- Pages, F., Dautel, H., Duvallet, G., Kahl, O., de Gentile, L., & Boulanger, N. (2014). Tick repellents for human use: prevention of tick bites and tick-borne diseases. Vector Borne and Zoonotic Diseases (Larchmont, N.Y.), 14(2), 85–93. https://www.doi.org/10.1089/vbz.2013.1410
- Swai, J. K., Soto, A. C., Ntabaliba, W. S., Kibondo, U. A., Ngonyani, H. A., Mseka, A. P., . . . Moore, S. J. (2023). Efficacy of the spatial repellent product Mosquito Shield™ against wild pyrethroid-resistant Anopheles arabiensis in south-eastern Tanzania. Malaria Journal, 22(1), 249. https://www.doi.org/10.1186/s12936-023-04674-4
